Abstract
Background: Social determinants of health including race and ethnicity, and socioeconomic status, are associated with many adverse health outcomes including mortality in the United States (US). Little is known on their relationship with treatment and course of acute pulmonary embolism (PE) in in the US.
Purpose: To study associations of social determinants of health with hospital management and fatality of hospitalized PE.
Methods: We identified all hospitalizations of adults with a discharge diagnosis of acute PE from the Nationwide Inpatient Sample (NIS; 2016-2018). A subgroup of high-risk PE was defined based on codes for shock, ventilator support, cardiac arrest, cardiopulmonary resuscitation, or vasopressor use. Multivariable logistic regression was used to study associations of race and ethnicity, type of primary payer, and income with use of "advanced PE therapy" (defined as thrombolysis, catheter directed treatment, surgical embolectomy, or extracorporeal membrane oxygenation) and in-hospital death.
Results: 1,124,204 PE hospitalizations (615,570 with primary diagnosis of PE) were identified. There were 66,570 patients (5.9%) with high-risk PE. The PE hospitalization rate for US adults was 14.9/10,000 person-years, increasing across race and ethnicity groups: 3.0 (95% CI 2.9-3.1) in Asian people, 5.6 (95% CI 5.4-5.7) in Native American people, 6.0 (95% CI 5.9-6.1) in Hispanic people, 13.1 (95% CI 13.1-13.2) in White people, and 20.1 in Black people (95% CI 20.0-20.2).
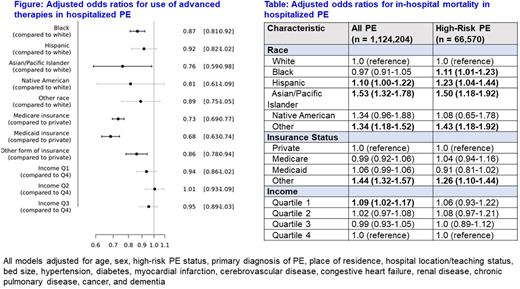
Advanced PE therapy was used in 5.5% of all patients, and 19% of those with high-risk PE. Compared with White patients, adjusting for other factors, Black patients were 13% less likely to receive advanced therapy, and Asian patients were 24% less likely to receive this (Figure). Compared to privately-insured patients, Medicare-insured patients were 27% less likely, Medicaid-insured patients were 32% less likely, and "other-insured" (includes uninsured) were 14% less likely to receive these treatments. Patterns were similar in people with high-risk PE (not shown).
Case-fatality in hospital for all PE patients was 6.4%, and for high-risk PE 50% died. The Table shows that Hispanic patients had 10% greater mortality than White patients, and Asian patients had 50% greater mortality; those with the lowest income had 9% greater mortality. Among high-risk PE patients, Black, Hispanic and Asian patients had 11-50% greater mortality than White patients, independent of other factors. For insurance status, "other-insured" patients in both PE groups had greater mortality than privately-insured patients.
Conclusion: We observed racial inequity in use of advanced therapies for acute PE, and higher in-hospital mortality in non-White than White patients in the US. Lower socioeconomic status measures were also associated with less use of advanced therapies and greater in-hospital mortality. Reasons for these social inequities in PE management and outcomes require study.
Disclosures
Giannakoulas:Bayer HealthCare: Consultancy, Other: Lecture fees; Pfizer: Consultancy, Other: Lecture fees; LeoPharma: Consultancy, Other: Lecture fee. Hobohm:MSD: Consultancy, Other: Lecture fees. Piazza:Bristol-Myers Squibb/Pfizer Alliance: Consultancy, Research Funding; Bayer: Research Funding; Janssen: Consultancy, Research Funding; Alexion: Research Funding; Amgen: Consultancy, Research Funding; Boston Scientific Corporation: Consultancy, Research Funding; Namsa: Consultancy; Prairie Education and Research Cooperative: Consultancy; Boston Clinical Research Institute: Consultancy. Konstantinides:Bayer AG: Consultancy, Honoraria; Daiichi-Sankyo: Consultancy; Boston Scientific: Consultancy; Inari Medical: Honoraria; MSD: Honoraria; Pfizer: Honoraria; Bristol-Myers Squibb: Honoraria. Barco:Bayer: Honoraria, Research Funding; Sanofi: Research Funding; Boston Scientific: Honoraria, Research Funding; Medtronic: Research Funding; Inari: Honoraria, Other: Data Safety Monitoring Board or Advisory Board ; Concept Medical: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.